INTRODUCTION
Uterine fibroid is a benign or non-cancerous growth of the smooth muscles of the uterus. They occur during the reproductive years of a woman and usually will begin to shrink after menopause. They usually do not cause any challenge in most women and are usually incidental findings during an ultrasound scan.
As many as 4 in 10 women may have fibroids in any population, and by age 50 years about 70 – 80 % of women will be found to have fibroids. Several factors may increase a woman’s risk of developing fibroids. These include:
- a family history of uterine fibroids in sisters, mother or aunts,
- being a black woman increases your risk,
- overweight women
SYMPTOMS
Most persons with fibroids have no symptoms. When symptoms occur, the client complains of:
- Shifting abdominal mass. Most women describe it as regular movements within the abdomen.
- Heavy menses with the use of additional pads
- Abdominal pains during menses
- Difficulty urinating [if the fibroid is compressing on the lower part of the urinary bladder]
LOCATION OF FIBROIDS
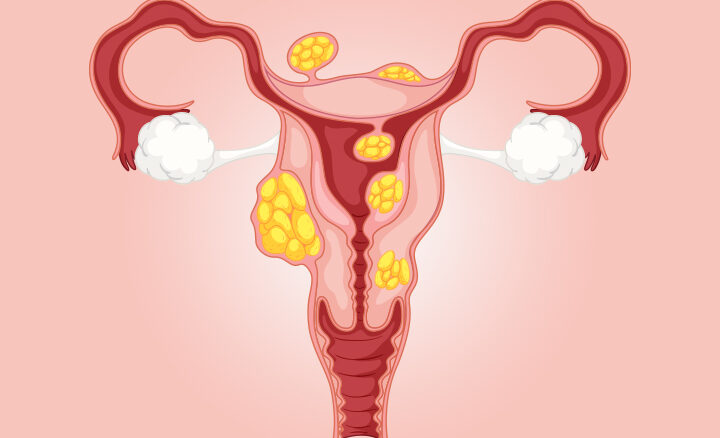
The location of a fibroid could determine if a fibroid would cause symptoms. The different locations include:
- Intramural fibroids
They are located in the muscular walls of the fibroid and may enlarge inwards or outwards. Small intramural fibroids generally do not cause symptoms.
- Submucosal fibroids
These are protrusions of fibroid into the uterine cavity thus distorting it and increasing its surface area for bleeding. They usually cause heavy bleeds.
- Subserosal fibroids
They are located on the external surface of the uterus.
- Pedunculated fibroids
These are fibroids that grow outside the surface of the uterus and develop a stalk.
- Cervical fibroids
They are located in the wall of the cervix (neck of the uterus).
- Parasitic fibroids
These fibroids are usually pedunculated and then develop blood vessels from other structures
CAUSES
The exact reason why women develop fibroid is still unknown. Factors that increase a woman’s risk include:
- Genetic factors
Fibroid tends to run in families and is common in families where a mother or aunt is found to have fibroids. It is also commoner in black women.
- Obesity
Fibroids are more common in obese women because of the conversion of fat to estrogen. Fibroids feed on estrogen for their growth.
PREVENTION
There are no ways of preventing uterine fibroids as most cases have a genetic potential. However, you may be able to reduce your risk slightly by maintaining a normal weight.
Regular check-ups with your gynaecologist are necessary if you have been diagnosed with uterine fibroids to monitor the growth of the fibroids.
COMPLICATIONS
Fibroids are benign tumours and do not pose any long term dangers to a woman. However, they could cause the following:
- Anaemia
A heavy menstrual flow could lead to blood loss and low blood levels. In some cases, the lady may need a blood transfusion.
- Dysmenorrhea
Painful menses could affect the quality of life of the client by causing severe pains during menses.
- Infertility
Fibroids rarely are a cause of infertility except in rare cases when it occludes both fallopian tubes.
- Recurrent pregnancy losses
If a pregnancy implants on a submucous fibroid, it could lead to pregnancy loss.
- Pregnancy challenges
Women who get pregnant with fibroids could be at risk of pains during the 2nd trimester of pregnancy [when the fibroid undergoes degeneration], poor growth of the developing baby, preterm delivery and heavy bleeding after delivery.
DIAGNOSIS
Diagnosing uterine fibroid usually begins with a history of abdominal swelling or heavy menses. However, in many cases, it is picked up during a routine pelvic examination or an ultrasound scan for another medical condition.
The pelvic examination usually reveals a pelvic mass.
Laboratory tests may be required and examination done may include:
- Full blood count. This checks for the presence of anaemia [low blood level], and the platelet count. It could assist in detecting blood disorders.
- Clotting profile. It helps to check for problems with blood clotting.
A 3D ultrasound scan will help confirm the diagnosis including the numbers of fibroids and their location.
Hysterosonography which uses saline to expand the endometrial cavity helps make a diagnosis of submucous fibroid.
MRI may be indicated when planning for treatment or surgery for women with large fibroids to get more details about the sizes and location of the fibroid, to ascertain that they are not cancerous.
TREATMENT
When a doctor makes a diagnosis of uterine fibroid, the plan to treat will be determined by the symptoms. Modalities of treatment include:
Expectant management
Women without symptoms usually do not require any treatment. They are counselled to have regular checkups.
Medical Treatment
Medications are used for the treatment of some of the symptoms of fibroids or to temporarily reduce the size of the fibroids. They include:
- These drugs are used to relieve painful menses. Examples are Ibuprofen, Brustan, Cataflam.
- Mefenamic acid. Used to reduce the amount of bleeding during menses.
- Oral contraceptive pills. They are used to reduce the amount of menstrual flow.
- Mirena [progesterone IUD]. This is an insert implanted into the uterus to reduce menstrual blood flow.
- GnRH agonist. They are injections used to induce a state of reversible menopause in a woman thus temporarily shrinking the fibroids and reducing blood flow. They are used for a maximum of 6 months. They are also used to make fibroids smaller before a planned surgery.
Uterine Artery Embolization [UAE]
It is used in women who do not desire to get pregnant. UAE involves inserting some gel into the uterine artery through a catheter to block the uterine artery blood flow to the uterus. The fibroids will shrink over months following the procedure.
Surgery
- Myomectomy
This involves the removal of the fibroids in women who still desire to have babies in the future. Fibroids could be removed through:
- Laparoscopic myomectomy
Laparoscopy is the preferable method for fibroid removal. It is done by inserting a camera through a pinhole and the instruments for surgery are inserted through small holes on the abdomen. The fibroids are removed by morcellation [a procedure which cuts it into smaller pieces so it can be pulled out of the small incisions]
- Hysteroscopic myomectomy
For submucous fibroids, removal can be carried out successfully through the vaginal route without making any incisions on the abdomen.
- Laparotomy or abdominal myomectomy
This is the traditional method of removing fibroids. It is used for large fibroids or multiple fibroids when laparoscopic removal is not feasible.
Hysterectomy
This involves the removal of the uterus for women who are no longer interested in childbearing. It could be carried out laparoscopically or via open surgery.
WHEN TO SEE A DOCTOR
You are advised to see your doctor if you experience the following.
- If you have heavy menses lasting for more than 7 days
- If you have painful menses
- If you notice your abdomen is increasing in size
- If you have had an ultrasound scan that revealed uterine fibroids